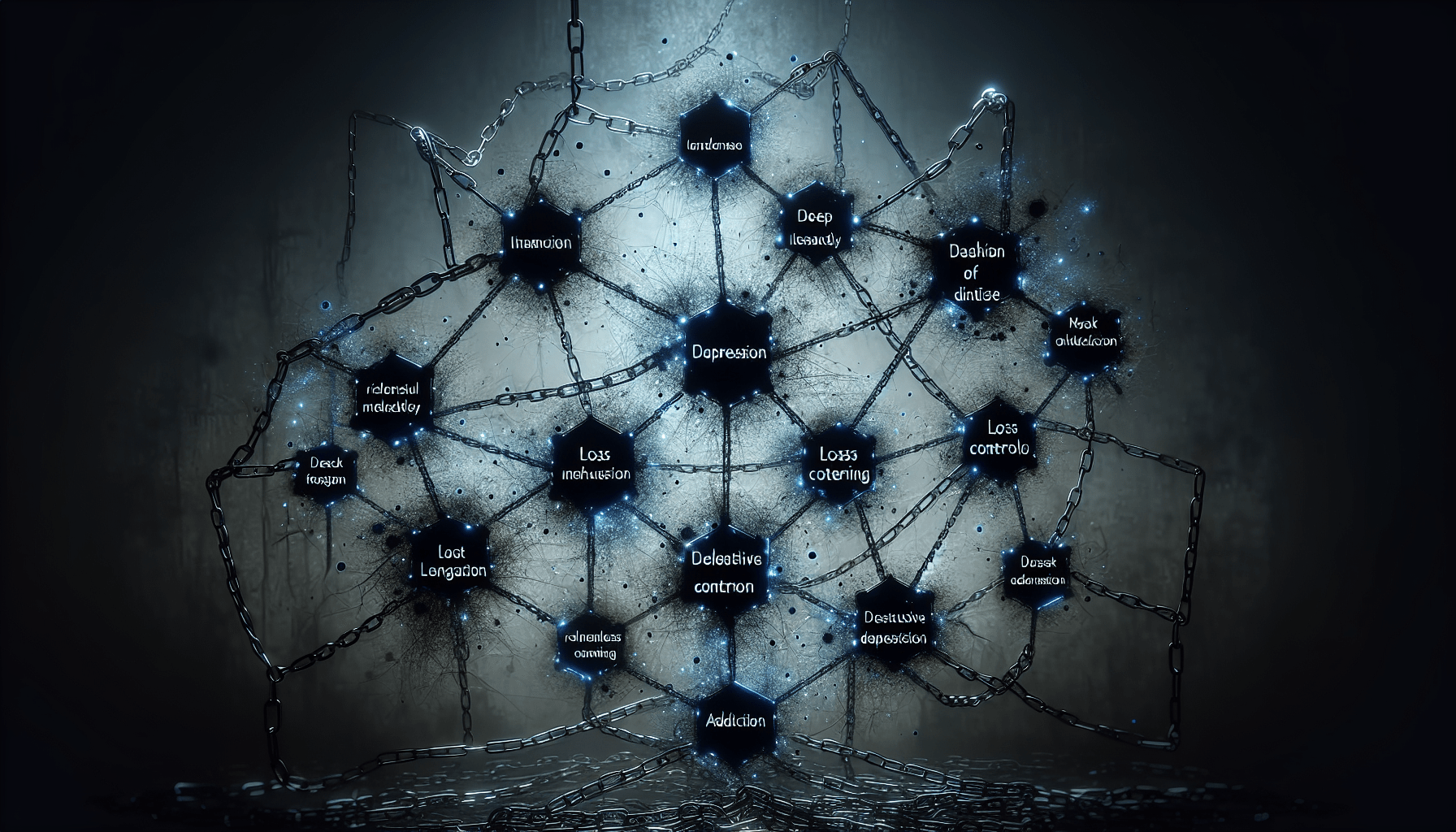
Depression is a complex and often misunderstood mental health condition that can have a profound effect on individuals’ lives. But here’s an intriguing thought: can depression itself become addictive? This article explores the notion of whether depression, with its all-consuming grip on one’s emotions and thoughts, has the potential to become a sort of addictive cycle. By examining the psychological and physiological aspects of depression, we aim to shed light on this intriguing concept and provide a fresh perspective on the intricate relationship between depression and addiction.
Overview of Depression
Understanding Depression
Depression is a common mental health condition that affects millions of people worldwide. It is characterized by a persistent feeling of sadness, hopelessness, and a loss of interest in activities that were once enjoyed. Despite its prevalence, depression is often misunderstood and stigmatized, making it important to educate yourself about this condition.
Symptoms of Depression
Depression can manifest in various ways, and it’s vital to recognize the symptoms to seek appropriate help. Some common symptoms of depression include persistent feelings of sadness or emptiness, loss of interest or pleasure in activities, changes in appetite or weight, sleep disturbances, fatigue or loss of energy, feelings of guilt or worthlessness, difficulty concentrating or making decisions, and recurrent thoughts of death or suicide. It’s important to remember that everyone’s experience with depression may be unique, but these symptoms can serve as a guide.
Causes of Depression
Depression does not have a single cause, as it is a complex condition influenced by various factors. Biological factors, such as imbalances in brain chemistry or genetics, play a role in predisposing individuals to depression. Environmental factors, such as traumatic life events, chronic stress, or a history of abuse, can also contribute to the development of depression. Additionally, certain personality traits and a family history of depression may increase an individual’s susceptibility. It’s essential to understand that depression is not solely a result of personal weakness or character flaws, but rather a combination of multiple factors.
Addiction and Its Characteristics
Understanding Addiction
Addiction is a chronic brain disease characterized by compulsive drug use or engagement in activities despite negative consequences. It involves a complex interplay of genetic, environmental, and behavioral factors. Addiction is not limited to substance abuse; it can also manifest as behavioral addictions, such as gambling or compulsive internet use. Understanding addiction is crucial to recognize the similarities and connections between addiction and depression.
Types of Addictions
Addictions can encompass various substances or behaviors, each with its distinctive characteristics. Substance addictions involve the excessive use of drugs or alcohol, while behavioral addictions include activities such as gambling, gaming, or shopping. Both substance and behavioral addictions can have significant physical, psychological, and social consequences for individuals. It’s important to acknowledge that addiction does not discriminate and can affect individuals from all walks of life.
Characteristics of Addiction
Addiction is characterized by several distinct features. These include an intense craving or urge to engage in the addictive behavior, loss of control over the behavior, continued use despite negative consequences, and withdrawal symptoms when the behavior is discontinued. Addiction also encompasses tolerance, where individuals require increasing amounts of the substance or engagement in the behavior to achieve the desired effect. Understanding these characteristics can help shed light on the complex nature of addiction and its relationship with depression.
Link Between Depression and Addiction
Prevalence of Co-occurring Depression and Addiction
There is a significant connection between depression and addiction, with both often co-occurring in individuals. Research has shown that approximately one-third of individuals with a substance use disorder also experience symptoms of depression. The coexistence of depression and addiction can complicate the treatment process and increase the risk of relapse. Recognizing the prevalence of this comorbidity is essential for developing effective treatment strategies.
How Depression Can Lead to Addiction
Depression can act as a contributing factor to the development of addiction. Many individuals with depression turn to substances or behaviors as a means of self-medicating or escaping from emotional pain. The temporary relief provided by substances or engaging in addictive behaviors may create a sense of comfort or numbness. However, this self-medication can quickly escalate into a full-blown addiction, as individuals rely on these substances or behaviors to cope with their depressive symptoms.
How Addiction Can Exacerbate Depression
On the other hand, addiction can worsen symptoms of depression and contribute to a vicious cycle. Substance abuse can disrupt the brain’s natural chemistry, leading to imbalances in neurotransmitters such as dopamine and serotonin, which are crucial for regulating mood and emotions. As a result, individuals may experience increased feelings of depression, anxiety, or even suicidal thoughts. Additionally, the negative consequences that often accompany addiction, such as strained relationships or financial difficulties, can further exacerbate depressive symptoms.
Depression as a Coping Mechanism
Depression as an Escape
For some individuals, depression can serve as a way to escape from overwhelming emotions or stressful situations. The act of withdrawing from the world, isolating oneself, and retreating into a depressive state may provide a temporary respite from external stressors. However, this coping mechanism ultimately perpetuates the cycle of depression and can lead to further negative consequences, such as worsening relationships or detachment from fulfilling experiences.
Depression as Self-Medication
Depression can also be viewed as a form of self-medication. Some individuals may unconsciously use depressive symptoms to dampen emotional pain or numb themselves from intense feelings. The temporary relief obtained from this mechanism reinforces the behavior, making it difficult to break the cycle. Recognizing depression as a maladaptive coping strategy is vital for exploring healthier alternatives and seeking appropriate treatment.
Depression as a Cycle
Depression and addiction can create a cyclical pattern, with each condition feeding into the other. Depression may initially lead to addiction as a coping strategy, while addiction further perpetuates and intensifies depressive symptoms. This cycle can be challenging to break without proper intervention and support. Understanding this interplay is crucial when developing effective treatment strategies for individuals experiencing both depression and addiction.
Neurobiology of Depression and Addiction
Similarities in Brain Circuitry
Both depression and addiction have been associated with alterations in the brain’s reward circuitry. The reward circuit involves the release of neurotransmitters, particularly dopamine, which plays a crucial role in regulating pleasure and motivation. In individuals with depression or addiction, this circuit can become dysregulated, leading to reduced dopamine activity or altered responsiveness to rewards. These shared neurobiological mechanisms contribute to the overlapping nature of depression and addiction.
Dopamine and Serotonin Imbalance
Imbalances in neurotransmitters, particularly dopamine and serotonin, have been implicated in both depression and addiction. Decreased levels of dopamine and serotonin are often observed in individuals with depression, contributing to the characteristic symptoms of low mood and anhedonia. Similarly, addictive substances or behaviors can stimulate the release of dopamine, leading to feelings of pleasure or reward. However, chronic substance abuse can deplete these neurotransmitters over time, exacerbating depressive symptoms and reinforcing addictive behaviors.
Role of Reward Pathways
The reward pathway in the brain, which involves the release of dopamine, plays a significant role in both depression and addiction. This pathway is responsible for reinforcing pleasurable experiences and motivating behaviors that are essential for survival. In individuals with depression, this pathway may be impaired, leading to reduced feelings of pleasure and motivation. Conversely, addictive substances or behaviors can hijack this pathway, creating an artificial sense of reward and reinforcing compulsive behaviors. Understanding the role of reward pathways can help inform treatment approaches that target these underlying mechanisms.
Treatment Approaches
Integrated Treatment for Dual Diagnosis
When treating individuals with co-occurring depression and addiction, an integrated approach is crucial. Integrated treatment involves addressing both conditions simultaneously, recognizing their interdependency and tailoring interventions accordingly. This approach can involve a combination of therapy, medication, and support systems to address both the psychological and physiological aspects of depression and addiction. By treating both conditions concurrently, individuals have a better chance of achieving long-term recovery.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a widely used therapeutic approach that has shown efficacy in treating both depression and addiction. CBT aims to identify and modify negative thought patterns and behaviors that contribute to depressive symptoms or addictive behaviors. By challenging distorted thinking and replacing maladaptive coping strategies with healthier alternatives, individuals can develop more adaptive ways of managing their emotions and overcoming addictive tendencies.
Medication and Pharmacological Interventions
In some cases, medication may be necessary to support individuals with co-occurring depression and addiction. Antidepressant medications can help stabilize mood and alleviate depressive symptoms, while other medications may be prescribed to manage substance cravings or withdrawal symptoms. Pharmacological interventions should be administered under the supervision of a qualified healthcare professional and complemented by therapy and support systems to address the holistic needs of individuals.
Addressing Co-occurring Disorders
Recognizing the Need for Dual Diagnosis Treatment
Recognizing the presence of co-occurring disorders, such as depression and addiction, is crucial for providing appropriate treatment. Both conditions have unique challenges and require tailored interventions to address their specific needs. By identifying the presence of co-occurring disorders, healthcare professionals can design comprehensive treatment plans that consider the complex interplay between depression and addiction.
Integrated Treatment Programs
Integrated treatment programs provide an essential framework for addressing co-occurring disorders. These programs often involve a multidisciplinary team of healthcare professionals, including counselors, therapists, and medical doctors, who collaborate to provide comprehensive care. Integrated treatment programs offer a range of therapeutic interventions, such as individual counseling, group therapy, family therapy, and educational workshops, to address both the psychological and physiological aspects of depression and addiction.
Importance of Supportive Environment
Creating a supportive environment is crucial for individuals seeking recovery from depression and addiction. Support systems can include family members, friends, support groups, and mentors who provide understanding, encouragement, and accountability. Supportive environments foster a sense of belonging, reduce feelings of isolation, and provide individuals with the resources and encouragement needed to sustain their recovery efforts.
Breaking the Cycle
Identifying Triggers and Risk Factors
Breaking the cycle of depression and addiction involves identifying triggers and risk factors that contribute to the onset or escalation of symptoms. Triggers can be environmental, social, or emotional factors that evoke negative emotions or cravings for substances or addictive behaviors. Recognizing these triggers allows individuals to develop strategies for managing and avoiding them, reducing the likelihood of relapse and promoting healthier coping mechanisms.
Developing Healthy Coping Mechanisms
Developing healthy coping mechanisms is a vital aspect of breaking the cycle of depression and addiction. Instead of relying on self-destructive behaviors, individuals can learn and practice healthier ways of managing stress, emotions, and challenging situations. This may involve engaging in activities that promote relaxation, such as mindfulness or meditation, pursuing hobbies or interests, seeking support from loved ones, or engaging in therapy or counseling to develop effective coping strategies.
Building a Support Network
Building a support network is essential for sustaining recovery and breaking the cycle of depression and addiction. Support networks can consist of friends, family, support groups, or mentors who provide guidance, understanding, and encouragement. These individuals can offer accountability, serve as a sounding board during challenging times, and provide the necessary emotional support needed for long-term recovery.
Holistic Approaches to Healing
Mindfulness and Meditation
Practicing mindfulness and meditation can be beneficial for individuals with co-occurring depression and addiction. Mindfulness involves intentionally focusing on the present moment, cultivating non-judgmental awareness of thoughts, feelings, and sensations. Meditation, on the other hand, involves training the mind to achieve a state of deep relaxation and heightened awareness. These practices can reduce stress, promote emotional well-being, and enhance self-awareness, allowing individuals to better navigate the challenges of recovery.
Exercise and Physical Well-being
Engaging in regular exercise and prioritizing physical well-being can have a positive impact on both depression and addiction recovery. Exercise has been shown to improve mood, boost self-esteem, and reduce symptoms of depression. Additionally, physical activity releases endorphins, the body’s natural feel-good chemicals, providing a natural way to experience pleasure and reward. Adopting a healthy lifestyle that includes regular exercise and proper nutrition can support overall well-being and enhance the recovery process.
Self-care and Self-compassion
Self-care and self-compassion are essential components of healing from depression and addiction. Individuals must prioritize their own well-being and engage in activities that nourish their mind, body, and spirit. This may involve setting healthy boundaries, practicing self-care rituals, engaging in activities that bring joy and fulfillment, and cultivating self-compassion by treating oneself with kindness and understanding. By prioritizing self-care, individuals can better manage stress, reduce symptoms of depression, and sustain their recovery efforts.
Recovery and Relapse Prevention
Importance of Recovery Support
Recovery support is crucial for individuals navigating the journey of overcoming depression and addiction. Recovery support systems can include professional therapists, support groups, peer mentors, and loved ones who provide guidance, encouragement, and accountability. These support systems can accompany individuals throughout their recovery journey, offering a safe space to share experiences, access resources, and receive ongoing support.
Relapse Prevention Strategies
Relapse prevention strategies play a vital role in maintaining long-term recovery from depression and addiction. It’s essential to identify high-risk situations and develop strategies to cope with cravings or potential triggers. This may involve utilizing healthy coping mechanisms, accessing support systems, implementing stress-management techniques, and actively engaging in self-care practices. By being proactive and vigilant, individuals can better navigate challenges and reduce the risk of relapse.
Continued Therapy and Aftercare
Continued therapy and aftercare are important components of maintaining recovery from depression and addiction. Therapy can provide ongoing support, help individuals address underlying issues, and develop strategies to manage relapse triggers. Aftercare programs, such as outpatient counseling or support groups, offer ongoing support and reinforcement of relapse prevention strategies. By engaging in continued therapy and aftercare, individuals can sustain their recovery efforts and build a fulfilling life in long-term sobriety.
In conclusion, depression and addiction are complex conditions that often co-occur and interact in intricate ways. Understanding the link between depression and addiction can help us recognize the importance of integrated treatment approaches and the need to address both conditions concurrently. By recognizing the unique characteristics, neurobiological similarities, and coping mechanisms of depression and addiction, we can develop comprehensive treatment strategies and support systems that promote recovery, well-being, and a hopeful future for individuals affected by these challenging conditions.