Imagine a world where we could understand the intricacies of our own minds, pinpointing exactly which part of our brain is responsible for the often debilitating condition of depression. This article seeks to uncover the mysteries behind this prevalent mental health disorder, exploring the specific region in the brain that scientists believe plays a significant role in its development. By shedding light on these neural pathways, we can strive towards a deeper understanding of the complex mechanisms that contribute to depression, ultimately paving the way for more effective treatments and interventions.
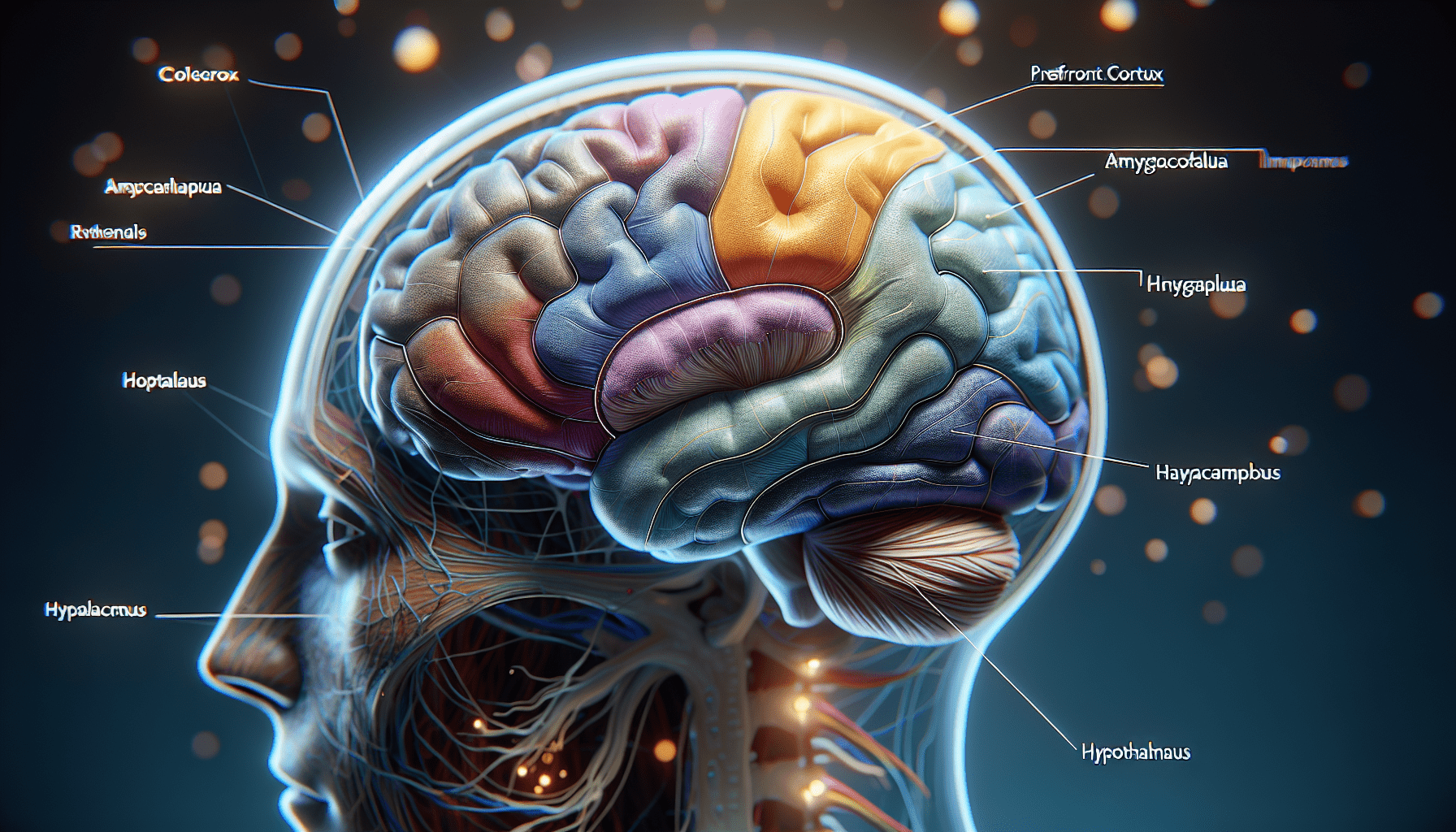
Prefrontal Cortex
Overview
The prefrontal cortex, located at the front of the brain, plays a crucial role in our emotional and cognitive functions. It is responsible for decision-making, problem-solving, planning, and regulating our emotions. The prefrontal cortex also helps us analyze risks and rewards, allowing us to make rational choices.
Role in Depression
In individuals with depression, the prefrontal cortex may exhibit abnormal activity and connectivity. Research suggests that people with depression often have reduced prefrontal cortex volume, leading to impaired cognitive and emotional processes. This could explain the difficulties in decision-making, problem-solving, and emotional regulation commonly experienced by those with depression.
Amygdala
Overview
The amygdala is an almond-shaped structure deep within the brain that plays a crucial role in processing emotions. It is responsible for detecting and interpreting emotional stimuli, particularly fear and threat responses. The amygdala also influences memory formation, learning, and attention.
Role in Depression
In individuals with depression, the amygdala may become overactive or hyper-reactive to negative emotional stimuli. This heightened emotional response can lead to feelings of sadness, anxiety, and fear. Over time, the repeated activation of the amygdala in response to negative events can contribute to the development and maintenance of depressive symptoms.
Hippocampus
Overview
The hippocampus is a seahorse-shaped structure located deep within the brain. It is primarily involved in memory formation and retrieval. The hippocampus also plays a crucial role in regulating our emotions and is connected to various areas of the brain involved in emotional processing.
Role in Depression
In individuals with depression, the hippocampus may undergo structural changes, including reduced volume and impaired functioning. These alterations can disrupt the regulation of emotions, leading to difficulties in mood regulation and memory formation. Additionally, a smaller hippocampus has been associated with an increased risk of developing depression.
Hypothalamus
Overview
The hypothalamus is a small but powerful structure located at the base of the brain. It serves as the control center for several essential bodily functions, including appetite, sleep, stress response, and the secretion of hormones. The hypothalamus also plays a vital role in regulating our emotions and is interconnected with various brain regions.
Role in Depression
In individuals with depression, the hypothalamus may exhibit dysregulation in the production and release of stress hormones and neuropeptides. These imbalances can lead to disrupted sleep patterns, changes in appetite, and abnormal responses to stress. The dysregulation of the hypothalamus can contribute to the manifestation and persistence of depressive symptoms.
Serotonin System
Overview
Serotonin is a neurotransmitter that plays a critical role in regulating mood, sleep, appetite, and other emotional processes. The serotonin system includes various brain regions, such as the prefrontal cortex, amygdala, and hippocampus, as well as the serotonin receptors.
Role in Depression
In individuals with depression, there may be an imbalance in serotonin levels or dysfunction within the serotonin system. This disruption can contribute to the development of depressive symptoms, including persistent low mood, reduced motivation, and disturbed sleep patterns. Medications that increase serotonin levels, such as selective serotonin reuptake inhibitors (SSRIs), are commonly used to treat depression.
Dopamine System
Overview
Dopamine is a neurotransmitter associated with reward, motivation, and pleasure. It plays a crucial role in regulating our emotional responses, motivation, and movement. The dopamine system includes several brain regions, including the prefrontal cortex, amygdala, and hypothalamus, as well as the dopamine receptors.
Role in Depression
In individuals with depression, there may be abnormalities in the dopamine system, leading to dysregulation of reward and motivation. This can result in reduced feelings of pleasure, decreased motivation, and anhedonia, which is the inability to experience pleasure from activities usually considered enjoyable. Medications that target the dopamine system, such as some antidepressants, may help alleviate these symptoms.
Norepinephrine System
Overview
Norepinephrine, also known as noradrenaline, is a neurotransmitter involved in regulating alertness, attention, and arousal. It plays a significant role in our stress response and mood regulation. The norepinephrine system includes various brain regions, such as the prefrontal cortex, amygdala, and hypothalamus, as well as the norepinephrine receptors.
Role in Depression
In individuals with depression, there may be an imbalance in the norepinephrine system, leading to reduced alertness, attentiveness, and low mood. Disruptions in this system can contribute to the fatigue, lack of energy, and difficulties in concentrating commonly experienced by those with depression. Some antidepressants target the norepinephrine system to improve these symptoms.
Brain-Derived Neurotrophic Factor (BDNF)
Overview
Brain-Derived Neurotrophic Factor (BDNF) is a protein that plays a vital role in the growth, development, and maintenance of neurons in the brain. It promotes the survival and formation of new connections between brain cells, allowing for optimal brain function. BDNF is involved in various processes, including memory, learning, and mood regulation.
Role in Depression
In individuals with depression, there may be a decrease in BDNF levels, leading to impaired neuroplasticity, which is the brain’s ability to adapt and change. Reduced BDNF levels can compromise the growth and maintenance of neurons, affecting brain regions involved in mood regulation. This disruption in neuroplasticity may contribute to the development and persistence of depressive symptoms.
Neurotransmitter Imbalance
Overview
Depression has been associated with imbalances in various neurotransmitters, including serotonin, dopamine, and norepinephrine. These imbalances can disrupt the communication between brain cells and affect mood, motivation, and emotional processes. The exact cause of these imbalances is still not fully understood, but they are believed to play a significant role in the development and progression of depression.
Role in Depression
Imbalances in neurotransmitters can contribute to the emergence of depressive symptoms. For example, low levels of serotonin or dopamine can lead to feelings of sadness, reduced motivation, and anhedonia. Similarly, abnormalities in norepinephrine levels can result in decreased alertness and attentiveness. Various medications used to treat depression aim to restore the balance of these neurotransmitters, helping alleviate depressive symptoms.
Genetics and Family History
Overview
Research suggests that genetics can predispose individuals to develop depression. Certain genetic variations can influence the way our brain processes and regulates emotions. Additionally, having a family history of depression increases the risk of developing the condition.
Role in Depression
Genetic factors contribute to approximately 40% of an individual’s risk for developing depression. Specific genes involved in neurotransmitter regulation, neuroplasticity, and stress response may increase susceptibility to depression. Understanding the genetic underpinnings of depression can help identify individuals at higher risk and develop personalized treatment approaches.
In conclusion, depression is a complex condition influenced by various brain regions, neurotransmitter systems, and genetic factors. The prefrontal cortex, amygdala, hippocampus, hypothalamus, serotonin system, dopamine system, norepinephrine system, BDNF, neurotransmitter imbalances, and genetics all play crucial roles in the development and manifestation of depression. By understanding the intricate mechanisms involved, researchers and clinicians can gain insights into effective treatment strategies and interventions for individuals struggling with depression.