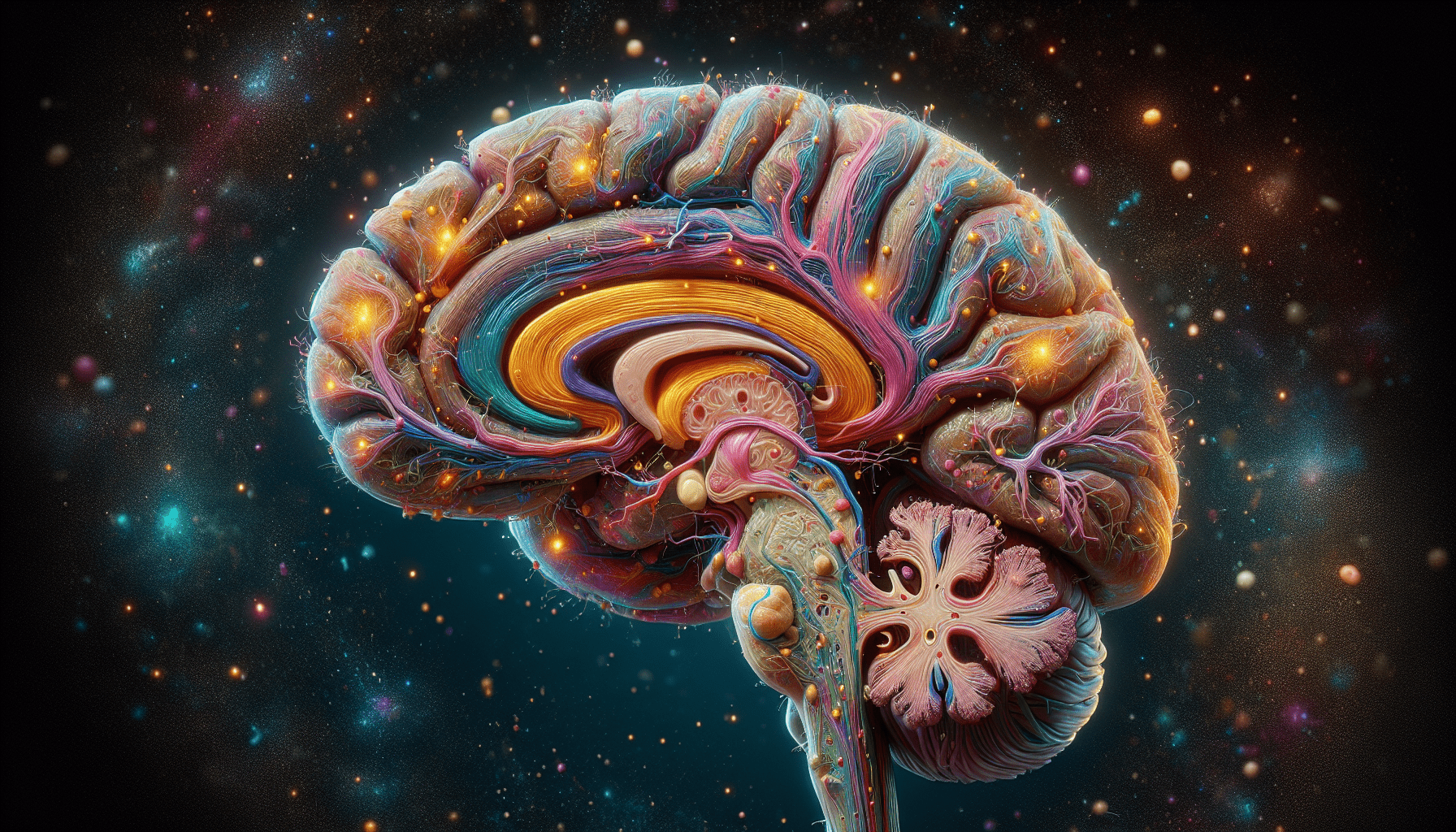
Welcome to an exploration of your brain and how it affects your emotions and mood! In this article, we will delve into the fascinating world of neuroscience to understand which specific part of your brain is responsible for controlling your emotions and potentially contributing to feelings of depression. By gaining a deeper insight into the intricate workings of our minds, we can ultimately learn how to better navigate and manage our mental health. Let’s embark on this enlightening journey together!
What Part Of The Brain Controls Emotion And Depression?
Have you ever wondered why you feel the way you do? Why some days you are filled with joy and happiness, while others you struggle to find any light in the darkness? The answer lies within your brain, specifically in the parts that control emotion and regulate mood. Let’s take a closer look at what part of the brain controls emotion and depression.
Understanding the Limbic System
The limbic system plays a crucial role in processing emotions and regulating mood. This complex network of structures in the brain includes the amygdala, hippocampus, and hypothalamus. The amygdala is responsible for processing emotional responses, the hippocampus helps form memories, and the hypothalamus regulates emotions and triggers the stress response.
The limbic system works in conjunction with other parts of the brain, such as the prefrontal cortex and the brainstem, to regulate emotions and mood. When this system is functioning properly, emotions are balanced, and mood is stable. However, disruptions in the limbic system can lead to emotional dysregulation and mood disorders like depression.
The Amygdala: The Emotional Center
The amygdala is often referred to as the emotional center of the brain. This almond-shaped structure is responsible for processing emotional responses, particularly fear and pleasure. When you experience a strong emotion, such as fear or joy, the amygdala sends signals to other parts of the brain to trigger a physiological response.
In individuals with depression, the amygdala may be hyperactive, leading to an exaggerated response to negative emotions and a decreased response to positive emotions. This can contribute to the persistent feelings of sadness and hopelessness that characterize depression.
The Hippocampus: Memory and Emotion
The hippocampus is another key structure in the limbic system that plays a crucial role in regulating emotion. This seahorse-shaped region of the brain is involved in forming memories and connecting them to emotions. In individuals with depression, the hippocampus may be smaller in size and have impaired function, leading to difficulties in processing emotional experiences and forming new memories.
The Hypothalamus: The Mood Regulator
The hypothalamus is a small but mighty structure located at the base of the brain that plays a crucial role in regulating emotions and triggering the stress response. This region of the brain is responsible for maintaining homeostasis, including regulating body temperature, hunger, and sleep. In individuals with depression, the hypothalamus may be overactive, leading to disruptions in the body’s stress response and circadian rhythms.
The Role of Neurotransmitters
Neurotransmitters are chemical messengers that transmit signals between neurons in the brain. These crucial molecules play a vital role in regulating mood, emotion, and behavior. In individuals with depression, imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine can contribute to the development of mood disorders.
Serotonin: The Happy Hormone
Serotonin is often referred to as the “happy hormone” due to its role in regulating mood, emotion, and sleep. This neurotransmitter plays a crucial role in modulating anxiety, depression, and aggression. In individuals with depression, serotonin levels may be low, leading to persistent feelings of sadness and hopelessness.
Dopamine: The Reward Neurotransmitter
Dopamine is often referred to as the “reward neurotransmitter” due to its role in the brain’s reward pathway. This crucial molecule is involved in regulating motivation, pleasure, and reward. In individuals with depression, dopamine levels may be low, leading to a decrease in motivation, feelings of worthlessness, and anhedonia (loss of interest in pleasurable activities).
Norepinephrine: Fight or Flight
Norepinephrine is a neurotransmitter that plays a crucial role in the body’s stress response. This molecule is involved in regulating alertness, arousal, and attention. In individuals with depression, norepinephrine levels may be dysregulated, leading to difficulties in concentration, mood swings, and irritability.
The Impact of Stress on the Brain
Stress is a normal and necessary part of life. However, chronic stress can have a detrimental impact on the brain, particularly on the parts that regulate emotion and mood. Prolonged exposure to stress can lead to structural changes in the brain, including a decrease in the size of the hippocampus and an increase in the activity of the amygdala.
The Hypothalamic-Pituitary-Adrenal (HPA) Axis
The hypothalamic-pituitary-adrenal (HPA) axis is a complex network of structures in the brain involved in regulating the body’s stress response. When you encounter a stressful situation, the hypothalamus releases corticotropin-releasing hormone (CRH), which triggers the release of adrenocorticotropic hormone (ACTH) from the pituitary gland. This, in turn, stimulates the release of cortisol from the adrenal glands.
In individuals with depression, the HPA axis may be overactive, leading to dysregulation of the stress response and increased levels of cortisol. Prolonged exposure to high levels of cortisol can have a detrimental impact on the brain, leading to structural changes in the hippocampus and amygdala.
Neuroplasticity and Depression
Neuroplasticity refers to the brain’s ability to reorganize itself in response to new experiences and changes in the environment. This remarkable process plays a crucial role in regulating mood, emotion, and behavior. In individuals with depression, disruptions in neuroplasticity can lead to structural changes in the brain that contribute to the development of mood disorders.
Structural Changes in the Brain
Chronic stress and depression can lead to structural changes in the brain, particularly in regions like the hippocampus and prefrontal cortex. The hippocampus may shrink in size, leading to difficulties in forming new memories and regulating emotions. The prefrontal cortex, which is involved in decision-making and impulse control, may also be affected, leading to difficulties in regulating mood and behavior.
Environmental Factors
Environmental factors, such as trauma, abuse, and neglect, can have a significant impact on the brain’s structure and function. Prolonged exposure to stressful or traumatic experiences can lead to changes in the brain that increase the risk of developing mood disorders like depression. However, positive experiences and interventions like therapy and medications can help promote neuroplasticity and improve mood and overall well-being.
Treatment Options for Depression
Depression is a complex and multifaceted disorder that requires a comprehensive approach to treatment. There are several treatment options available for individuals with depression, including therapy, medications, and lifestyle changes.
Therapy
Therapy, particularly cognitive-behavioral therapy (CBT) and interpersonal therapy, is a highly effective treatment for individuals with depression. These therapeutic approaches help individuals identify and challenge negative thought patterns, develop healthy coping mechanisms, and improve relationships with others. Therapy can help individuals understand the underlying causes of their depression and develop strategies to manage symptoms effectively.
Medications
Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), are commonly prescribed to individuals with depression. These medications work by increasing the levels of neurotransmitters like serotonin and norepinephrine in the brain, helping to regulate mood and reduce symptoms of depression. It is essential to work closely with a healthcare provider to find the right medication and dosage that works best for you.
Lifestyle Changes
Making positive lifestyle changes can have a significant impact on mood and overall well-being. Engaging in regular physical activity, practicing mindfulness and relaxation techniques, maintaining a healthy diet, and getting an adequate amount of sleep can help reduce symptoms of depression and improve quality of life. It is essential to prioritize self-care and seek support from loved ones and mental health professionals when needed.
In conclusion, the brain is a complex and intricate organ that plays a crucial role in regulating emotions and mood. Understanding the parts of the brain that control emotion and depression can help individuals recognize the signs and symptoms of mood disorders and seek appropriate treatment. By addressing imbalances in neurotransmitters, promoting neuroplasticity, and adopting healthy lifestyle habits, individuals can take steps to improve their emotional well-being and lead fulfilling lives. Remember, you are not alone, and help is available.