Have you ever wondered where MDD, or Major Depressive Disorder, comes from? This article aims to shed light on the origins of this debilitating condition, exploring the factors that contribute to its development and the impact it can have on individuals’ lives. By understanding the roots of MDD, we can gain valuable insights into effective treatment and support for those who are affected by it. Join us as we uncover the path that leads to this mental health challenge.
Genetic Factors
MDD, also known as Major Depressive Disorder, can have a genetic component. Family history plays a significant role in predisposing individuals to this condition. If you have a close family member such as a parent or sibling who has experienced depression, you may be more likely to develop MDD. Gene variants also contribute to the development of MDD. Certain genes that regulate mood, emotions, and stress responses may be different in individuals with depression compared to those without. These genetic factors can make someone more susceptible to experiencing depressive episodes.
Neurotransmitter Imbalances
Neurotransmitters are chemical messengers in the brain that play a crucial role in regulating our moods and emotions. Imbalances in specific neurotransmitters have been associated with MDD. Serotonin is one such neurotransmitter that is often linked to depression. Low levels of serotonin can contribute to feelings of sadness and low mood. Similarly, dopamine and norepinephrine imbalances can also play a role in the development of MDD.
Environmental Factors
While genetic factors and neurotransmitter imbalances can predispose individuals to MDD, environmental factors continue to play a significant role in its development. Childhood trauma, such as physical or emotional abuse, neglect, or the loss of a parent, can significantly increase the risk of developing MDD later in life. Chronic stress, whether related to work, relationships, or other life circumstances, can also contribute to the onset of depression. Additionally, experiencing a significant loss or bereavement can trigger depressive episodes in susceptible individuals.
Personality Traits
Certain personality traits have been associated with an increased likelihood of developing MDD. Negative thinking patterns, characterized by constant self-criticism, pessimism, and a tendency to focus on the negative aspects of life, can contribute to the development of depression. Perfectionism, or the constant striving for flawlessness and high standards, can also be a risk factor for MDD. Introversion, while not directly causing depression, can make individuals more vulnerable to social isolation, which can contribute to the development or exacerbation of depressive symptoms.
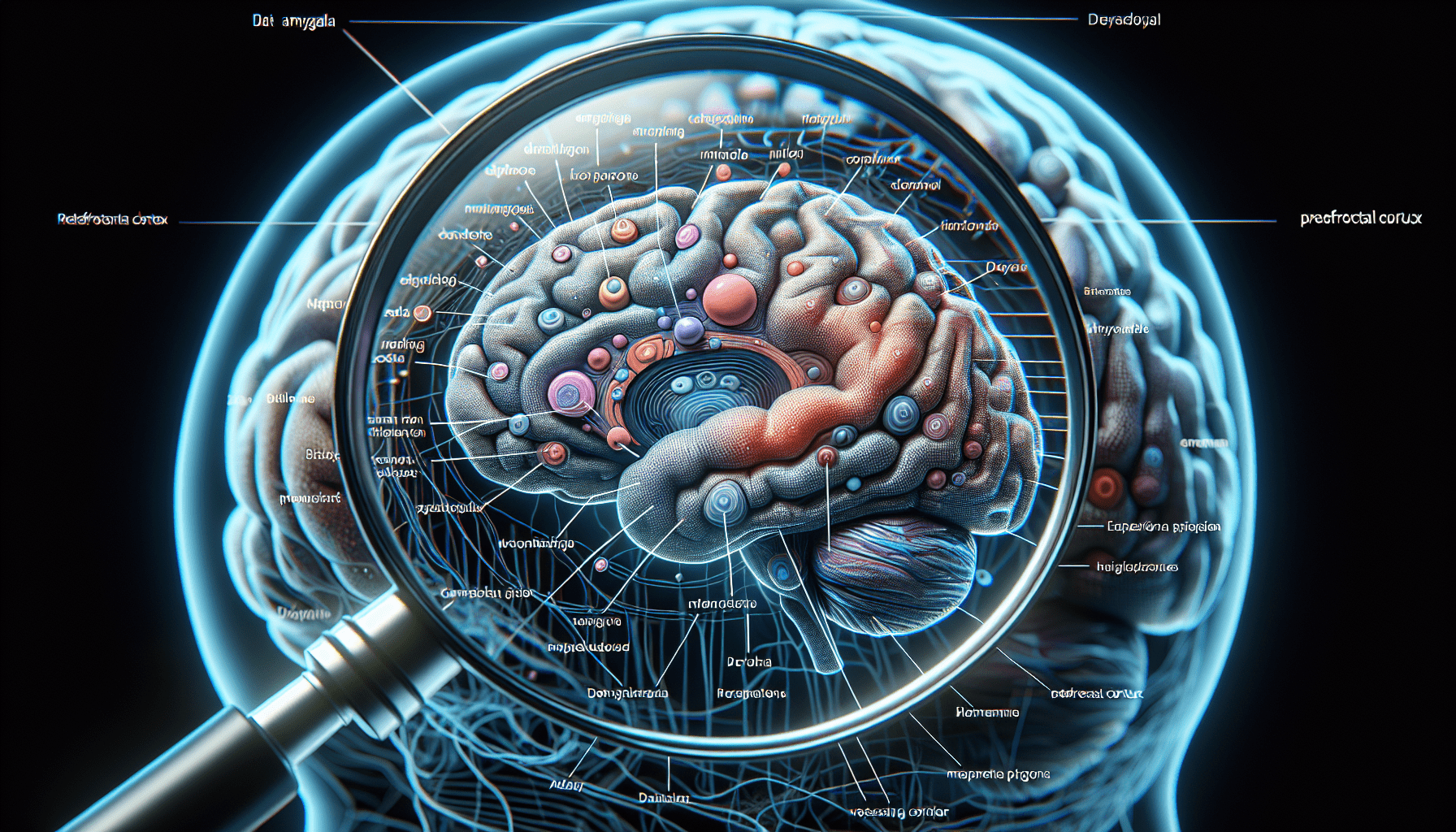
Brain Structure and Function
The structure and function of the brain can also play a role in the development of MDD. The amygdala, which is involved in processing emotions and regulating the stress response, may be overactive in individuals with depression. This heightened activity can contribute to increased feelings of fear, anxiety, and sadness. The prefrontal cortex, responsible for decision-making, impulse control, and emotional regulation, may also function differently in individuals with MDD. Additionally, the hippocampus, involved in memory and emotion regulation, may be smaller in people with depression.
Hormonal Factors
Hormonal imbalances can also influence the development of MDD. Thyroid hormones, which regulate metabolism and mood, can impact mental health when levels are too high or too low. Imbalances in sex hormones, such as estrogen and testosterone, have also been linked to depression. Changes in hormone levels during puberty, pregnancy, or menopause can contribute to the development of MDD or exacerbate existing symptoms.
Psychological Factors
Psychological factors and beliefs about oneself can contribute to the development of MDD. Low self-esteem, characterized by a negative self-image, constant self-criticism, and feelings of inadequacy, can make individuals more susceptible to depression. Body image issues, such as dissatisfaction with one’s appearance, can also contribute to feelings of worthlessness and depressive symptoms. Additionally, a sense of hopelessness or believing that life will never improve can contribute to the onset or persistence of depression.
Social Factors
Social factors can have a significant impact on mental health, including the development of MDD. Isolation, whether due to living alone, lack of social support, or feeling disconnected from others, can increase the risk of depression. Lack of supportive relationships, characterized by a lack of emotional support or understanding, can also contribute to the development or exacerbation of depressive symptoms. Discrimination based on race, gender, sexual orientation, or other factors can also contribute to the onset of MDD.
Medical Conditions
Certain medical conditions can increase the risk of developing MDD. Chronic illnesses, such as diabetes, cardiovascular disease, or autoimmune disorders, can contribute to feelings of sadness, hopelessness, and fatigue, which are common symptoms of depression. Additionally, painful conditions, such as fibromyalgia or chronic pain syndromes, can lead to the development or worsening of depressive symptoms.
Substance Abuse
Substance abuse, particularly alcohol and drug use, can significantly impact mental health and increase the risk of developing MDD. Alcohol is a depressant that can worsen depressive symptoms and increase the risk of developing a depressive disorder. Similarly, drug abuse, whether illicit substances or prescription medications, can alter brain chemistry, disrupt neurotransmitter balance, and contribute to the development or exacerbation of depression.
In conclusion, the development of Major Depressive Disorder (MDD) is influenced by a combination of genetic, environmental, and psychological factors. Genetic factors and neurotransmitter imbalances can make individuals more susceptible to developing MDD. Environmental factors, such as childhood trauma, chronic stress, and loss or bereavement, can trigger or exacerbate depressive symptoms. Personality traits, including negative thinking patterns, perfectionism, and introversion, can contribute to the development of MDD. Brain structure and function, hormonal imbalances, psychological factors, social factors, medical conditions, and substance abuse also play a role in the onset and persistence of MDD. Understanding these complex factors can help in developing effective prevention and treatment strategies for individuals struggling with MDD.