Welcome to an insightful article that explores the fascinating topic of the differences between a depressed brain and a normal brain. In this piece, you will gain a better understanding of the various ways in which the brain functions differently in individuals experiencing depression compared to those with a healthy mental state. By the end of this article, you will have a clearer picture of how depression affects the brain and the potential implications for treatment and management. Let’s delve into the complex world of neurology and mental health together!
What Is The Difference Between A Depressed Brain And A Normal Brain?
Hey there! Have you ever wondered what exactly is going on in the brain of someone with depression? Let’s dive into the fascinating world of neuroscience to explore the key differences between a depressed brain and a normal brain.
Neurotransmitters: The Messengers of the Brain
Neurotransmitters are like messengers in your brain, communicating vital information between brain cells. In depression, there is often an imbalance of these neurotransmitters, leading to disruptions in mood regulation.
Serotonin
Serotonin is often referred to as the “feel-good” neurotransmitter, playing a crucial role in regulating mood, sleep, appetite, and overall well-being. In depression, lower levels of serotonin are commonly observed, contributing to feelings of sadness and despair.
Dopamine
Dopamine is known as the “reward” neurotransmitter, responsible for feelings of pleasure and motivation. In depression, there may be decreased dopamine activity, leading to a lack of enjoyment in activities that were once pleasurable.
Norepinephrine
Norepinephrine is involved in the body’s response to stress, regulating heart rate, blood pressure, and mood. In depression, norepinephrine levels may be lower, contributing to symptoms such as fatigue and lack of motivation.
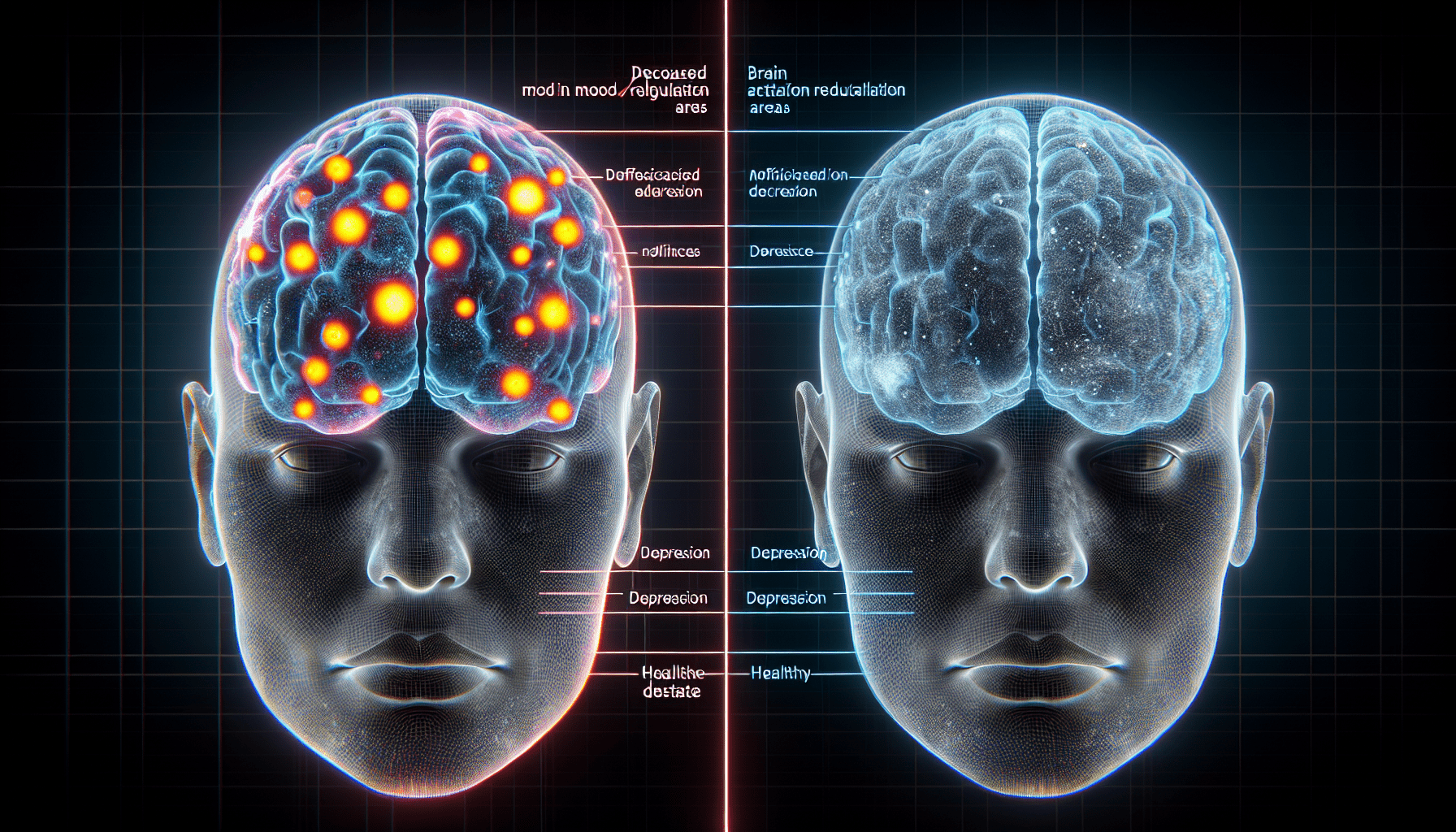
Brain Structure: The Anatomy of Depression
The structure of the brain can also be affected by depression, with specific regions showing differences in size, activity, and connectivity compared to a normal brain.
Hippocampus
The hippocampus is a key brain region involved in memory and emotion regulation. In depression, the hippocampus may shrink in size, affecting memory function and mood regulation.
Amygdala
The amygdala is responsible for processing emotions, particularly fear and pleasure. In depression, the amygdala may be overactive, leading to heightened feelings of anxiety and stress.
Prefrontal Cortex
The prefrontal cortex is crucial for decision-making, self-control, and emotional regulation. In depression, the prefrontal cortex may show decreased activity, impacting cognitive function and mood stability.
Neural Circuits: The Pathways of Depression
Neural circuits are like highways in the brain, allowing different regions to communicate and coordinate responses. In depression, disrupted neural circuits can lead to changes in mood, behavior, and cognition.
Default Mode Network
The default mode network is a set of brain regions that are active when the mind is at rest or engaged in introspection. In depression, there may be alterations in the default mode network, leading to rumination and negative self-talk.
Limbic System
The limbic system is a collection of brain structures involved in emotion, memory, and motivation. In depression, there may be dysfunction in the limbic system, resulting in mood disturbances and changes in motivation.
Reward Pathway
The reward pathway is responsible for processing pleasure and reinforcement. In depression, there may be reduced activity in the reward pathway, leading to decreased motivation and anhedonia (inability to feel pleasure).
Genetics: The Influence of DNA on Depression
Genetics can also play a significant role in the development of depression, with certain gene variations increasing susceptibility to the disorder.
SERT Gene
The SERT gene is involved in the regulation of serotonin levels in the brain. Variations in the SERT gene have been linked to an increased risk of depression, affecting how serotonin is reabsorbed and recycled in the brain.
BDNF Gene
The BDNF gene is responsible for producing brain-derived neurotrophic factor, a protein that promotes the growth and survival of neurons. Variations in the BDNF gene have been associated with depression, impacting brain function and plasticity.
COMT Gene
The COMT gene is involved in the breakdown of dopamine in the brain. Variations in the COMT gene have been linked to depression, affecting dopamine levels and neurotransmission.
Environmental Factors: The Impact of Your Surroundings
In addition to genetics, environmental factors can also contribute to the development of depression, influencing brain function and mental health.
Stress
Chronic stress can have a profound impact on the brain, altering neurotransmitter levels, shrinking brain regions, and disrupting neural circuits. Long-term exposure to stress can increase the risk of developing depression and other mental health disorders.
Trauma
Experiencing trauma, such as abuse, neglect, or loss, can have lasting effects on the brain, affecting emotional regulation, memory processing, and stress response. Trauma can increase susceptibility to depression and anxiety disorders.
Lifestyle
Your lifestyle choices, such as diet, exercise, sleep, and substance use, can also influence your mental health. A healthy lifestyle can support brain function, promote neurotransmitter balance, and reduce the risk of developing depression.
Treatment Options: Restoring Balance in the Brain
Fortunately, there are various treatment options available to help restore balance in the brain and alleviate symptoms of depression.
Medication
Antidepressant medications are commonly prescribed to rebalance neurotransmitters in the brain, such as serotonin, dopamine, and norepinephrine. These medications can help improve mood, reduce anxiety, and increase motivation.
Therapy
Cognitive-behavioral therapy (CBT) is a type of psychotherapy that focuses on changing negative thought patterns and behaviors associated with depression. Therapy can help you develop coping skills, improve self-esteem, and address underlying issues contributing to your depression.
Lifestyle Changes
Making positive lifestyle changes, such as exercising regularly, eating a balanced diet, getting enough sleep, and avoiding substance abuse, can support brain health and improve symptoms of depression. Physical activity, in particular, has been shown to boost neurotransmitter levels and enhance mood.
Conclusion: Understanding Depression from a Neuroscientific Perspective
Understanding the key differences between a depressed brain and a normal brain can shed light on the complex nature of depression and how it impacts brain function, structure, and connectivity. By exploring the role of neurotransmitters, brain structure, neural circuits, genetics, environmental factors, and treatment options, we can gain a deeper appreciation for the multifaceted nature of depression and the importance of personalized care in addressing mental health challenges. Remember, you are not alone in your journey towards mental wellness, and there are resources available to support you every step of the way. Take care of yourself and reach out for help when you need it. You deserve to feel your best and live a fulfilling life.